Virginia’s mental health hotline launches amid fears it won’t meet expectations
New 988 number, billed as part of the state’s crisis system expansion, won’t guarantee immediate access to services
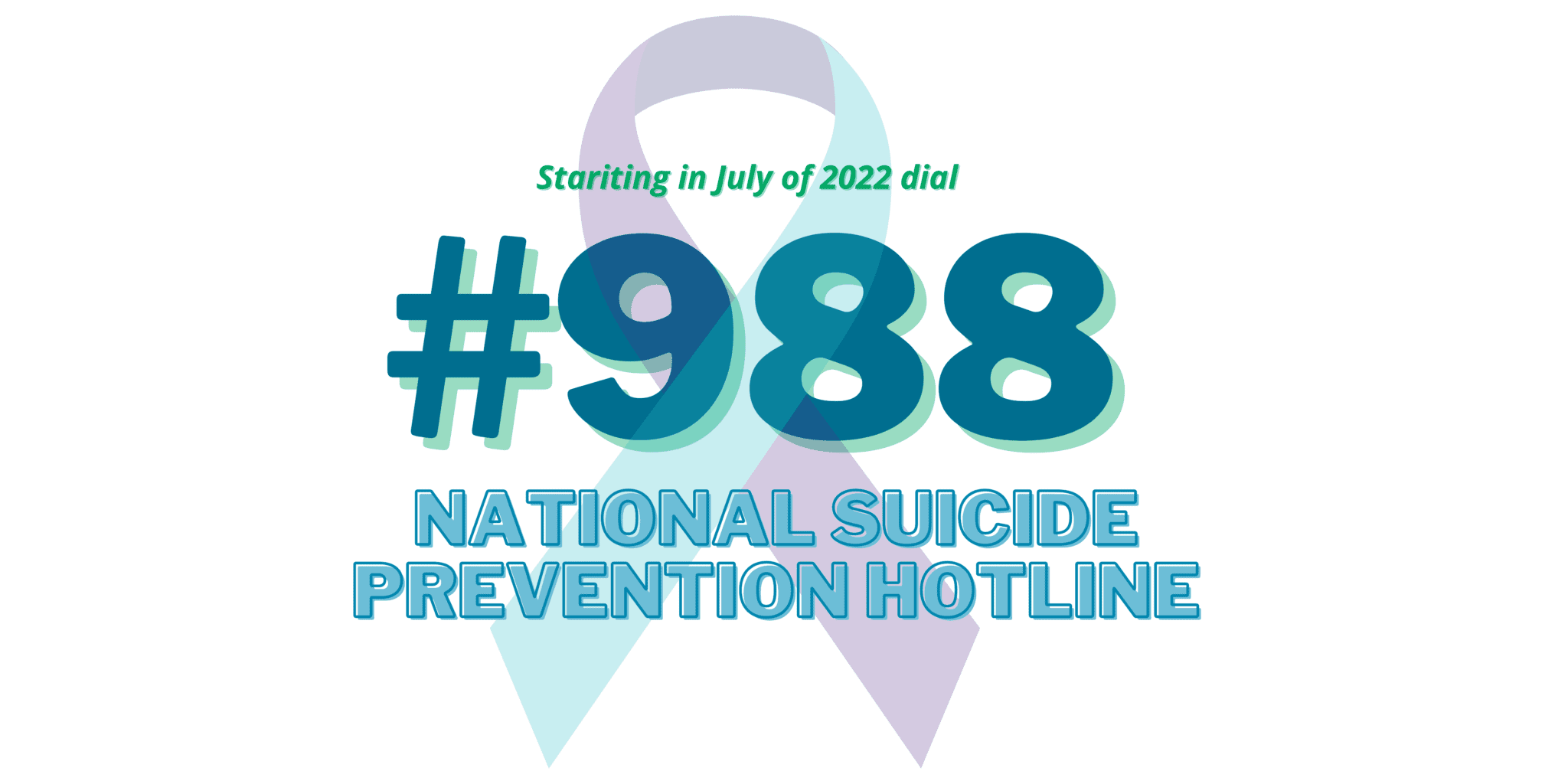
On Saturday, Virginia was part of a nationwide transition to 988, a simple three-digit hotline for mental health emergencies.
The new number replaced the National Suicide Prevention Lifeline, a longer — and harder to remember — 800 number that connected to a patchwork of local call centers across the country. The shift, which first began in Virginia last year, has already boosted call volumes by 25 percent and experts expect thousands more calls, texts and messages as awareness of the hotline grows across the state.
The centralized number is intended to streamline the current call-in process, making it far more likely that people will reach a responder on the first dial. But in Virginia, the hotline is also linked to the state’s build-out of crisis response services. Legislation that funded expanded call centers specifically listed the deployment of mobile crisis and community care teams as part of their duties and responsibilities. The ultimate goal is to dispatch trained providers out to calls that can’t be de-escalated over the phone, ideally within an hour after the call is received, said John Lindstrom, CEO of the Richmond Behavioral Health Authority.
However, the capacity to respond to those calls still varies widely across Virginia’s highly regionalized system of community service boards — the state and locally funded agencies tasked with providing crisis care services. Lindstrom said workforce shortages and varying funding levels have made hiring more challenging, preventing many CSBs from quickly scaling up those teams.
So while Virginia’s 988 call centers are fully up and running, there’s still wide variability in how quickly local agencies can launch a response — and what services they’re able to provide. Some mental health advocates worry it will confuse callers and potentially sow distrust in the system if people in crisis don’t receive the response they expect from the hotline, which some media outlets have described as “the mental health equivalent of 911.”
“I do have a concern there will be raised expectations,” said Bruce Cruser, executive director of the state’s affiliate of Mental Health America, an advocacy group for behavioral supports and services.
“The messaging has been confusing, not just in Virginia but throughout the country,” he continued. “And I think we should be clear that if you’re feeling suicidal or you’re in crisis, you can call 988 and you will be connected with a trained professional. But it does not mean you will immediately be able to connect with community resources.”
So, what can you expect from a hotline call?
While the state’s crisis response system is still in the development phase, its 988 call centers, in many ways, are ahead of the curve. Virginia was the first in the nation to implement a 988 service fee, funding the centers through a monthly telecom tax. And for months, the state’s Department of Behavioral Health and Developmental Services has been positioning two existing call centers — PRS in Northern Virginia and Frontier Health in Johnson City, Tennessee — to take on nearly 100 percent of mental health calls in Virginia.
“Between those two, what should occur is that calls with a Virginia area code get routed at the national level to either one of those call centers,” said Bill Howard, director of the agency’s Crisis Supports & Services division. PRS will be the primary call center for roughly 85 percent of the state, while Frontier will mostly handle communications from Southwest Virginia.
However, unlike 911, which routes callers to their nearest dispatch center through geolocation, the national 988 hotline routes are based on area code, warned Laura Clark, the senior director for PRS’ CrisisLink service. That means Virginians with out-of-state phone numbers likely won’t be connected to either call center — a problem federal officials are still working to address, she said.
But for in-state callers with Virginia area codes, the goal is to answer close to 100 percent of service calls within 20 seconds (PRS can also respond to texts and offers an online chat feature). Frontline agents typically aren’t licensed clinicians, but Clark said they’re trained to conduct preliminary assessments and offer emotional support to callers.
“There are just not enough clinicians in the world to man that front line,” she said. But if a caller does require a more intensive response, PRS has mental health professionals on staff to guide agents through the call and make sure they’re following protocols.
“Our first concern is a caller’s immediate safety — making sure they’re able to work through the call process because they’re not at imminent risk,” Clark continued. “We’re able to provide emotional support, help them create a plan for themselves, and then connect them to the behavioral health resource that helps match where their need is.”
Existing data from Tucson, Arizona, which has developed a robust crisis response system, indicate that call centers can resolve about 80 percent of crises without any further intervention, said Alyssa Ward, the behavioral health clinical director for Virginia’s Department of Medical Assistance Services. And when it comes to the 988 line itself, state officials are cautiously optimistic that Virginia’s system is prepared to handle an anticipated influx of new calls.
Clark said PRS is currently about 85 percent staffed and actively recruiting more agents. The state’s funding has also been enough to cover operational costs so far, though she warned that could change if call volumes continued to rise as significantly as they already have.
Howard also said that since January of last year, the in-state answer rate has increased by 33 percent, an encouraging sign that the call centers have been adjusting to increased demand. And the state is continuing to integrate more behavioral health services, including a potential tie-in with Mental Health America of Virginia’s warm line service for low-risk callers with questions about community resources or mental health recovery.
Still, there’s wide uncertainty over how prepared Virginia will be to provide services to callers whose needs aren’t met by frontline agents. The state is still in the process of building out a data platform intended to underpin the crisis system, allowing call centers and mobile crisis teams to access a statewide bed registry and comprehensive list of local community services.
Eventually, state officials are hoping to transition to a model similar to Tucson’s, frequently touted as a gold standard for the rest of the country. Under the system’s continuum of care, call centers are considered “traffic control” for a network of services, from its mobile crisis teams who can respond to patients 24 hours a day to stabilization centers where they can safely begin treatment.
But expanding those services statewide is a lofty goal, and one that’s already run into challenges. One of the biggest is a shortage of mental health providers, an existing problem in Virginia that experts say has only been exacerbated by the COVID-19 pandemic.
It’s become an even bigger concern as the state prepares for a surge in demand. Under Virginia’s developing crisis system, mobile teams will be sent out from five “regional hubs,” local dispatch centers operated by community service boards and equipped to handle higher-risk 988 calls. The intention, according to state planning, is to provide 24/7 access and response from a team within an hour.
Ultimately, Cruser said it all comes back to the need for more mental health treatment in Virginia. The current budget surplus has led to an infusion of cash for state hospitals and additional crisis receiving centers, among other services, but those are still in the early stages of development.
And as Virginia moves forward in some ways, it’s moved back in others. Earlier this year, for example, state lawmakers created an opt-out for the state’s recently implemented Marcus Alert system — another aspect of the crisis care continuum meant to reduce police involvement in mental health emergencies.
In practice, it means that more than half of the state’s 133 localities won’t be required to develop specialized co-response teams between mental health professionals and law enforcement agencies. There’s still a requirement for every city and county to develop a plan for referring mental health calls to the 988 hotline, but those protocols aren’t due until 2023, and officers could still be responding to behavioral health crises in much of Virginia for the foreseeable future if situations escalate before mobile providers can intervene.
Cruser worries it’s another aspect of the state’s rollout that could be confusing to callers, especially given that state officials have linked 988 to the Marcus Alert system and broader efforts to expand crisis services.
“What you don’t want is people expecting something from the hotline that they don’t get,” he said. “Then they’re less likely to use it. Particularly when we’re talking about a co-response or a clinical response to a mental health emergency instead of a police response.”
Virginia Mercury is part of States Newsroom, a network of news bureaus supported by grants and a coalition of donors as a 501c(3) public charity. Virginia Mercury maintains editorial independence. Contact Editor Robert Zullo for questions: info@virginiamercury.com. Follow Virginia Mercury on Facebook and Twitter.